Expertise
Over more than 15 years, I have acquired wealth of experience and knowledge. I hold specialist qualifications in several areas of gynaecology gained through the training programmes approved by Royal College of Obstetricians and Gynaecologists (RCOG).
More details for each skill is described below.
More details for each skill is described below.
-
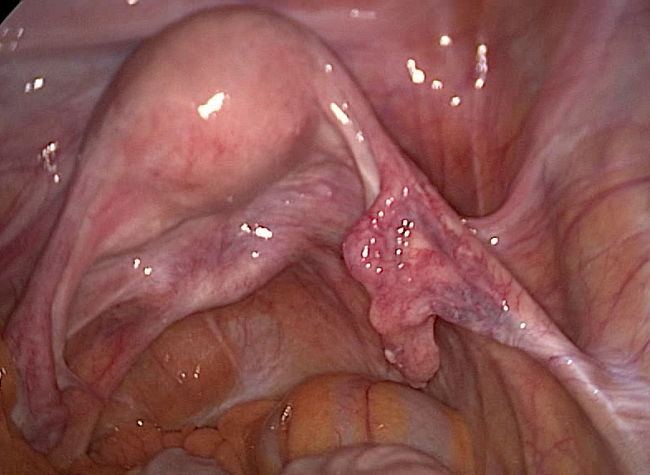
LaparoscopyLaparoscopy is one of the common procedure performed in gynaecology. It can be used for both diagnostic as well as treatment purposes. My specialist qualification and several years of complex laparoscopic surgery experience allows me to offer most of the surgical treatments with a laparoscopic approach. Only exception to this would be the large uterine or ovarian tumours (size more than 10cm).More information about laparoscopy is hereShow meWhat is laparoscopy?
Laparoscopy (also known as keyhole or minimally invasive) surgery allows a surgeon to perform operation inside the abdomen (tummy) and pelvis without having to make large incisions on the skin.
How is it performed?
Once patient is asleep with general anaesthetic antiseptic preparations are made. A small needle is then passed through umbilicus (belly button) and carbon dioxide gas is pumped to inflate the abdomen (tummy). Inflation of abdomen reduces the risk of injury and allows the surgeon a better visual field and space to perform procedures. slightly larger (5-10mm) trocars (tubes) are then inserted through small holes in abdominal wall, one of which is used to for the laparoscope and others for the laparoscopic instrument that performs the planned procedure. Laparoscope is attached with the light sources and relays the pictures to a television screen. Several highly specialised laparoscopic instruments are available to carry out specific jobs during the operation.
After the planned procedure is completed, surgeon will ensure that there is no bleeding and will let out the carbon dioxide. All small incisions are closed using dissolvable stitches. Patient is then awaken.
How long does it take?
Depending on the indication it could take 30min (simple diagnostic laparoscopy) to upto 5 hours for complex cancer operation (e.g. trachelectomy)
What are the advantages?- Shorter hospital stay and recovery time
- Less pain, bleeding and infection risk
- Cosmetically much less scarring
What are the disadvantages?
There are no real disadvantages of laparoscopic surgery compared to open surgery however…- Not all gynaecological operations can be done laparoscopically. For example large tumours involving ovaries or uterus usually requires incision.
- Also laparoscopic surgery requires a complex set of skills which are acquired by specific training, special interest and continued exposure of complex laparoscopic procedures. Compared to open surgery laparoscopic surgery requires additional skills to accommodate 3D orientation, understanding of tactile sensation through instrument, ergonomics of laparoscopy and energy used through instrument and above all additional safety precautions specific to laparoscopic procedures.
What are the risks and complications?
Laparoscopy in gynaecology is a commonly performed procedure and serious complications are rare.
Minor complications include:- Wound infection
- Minor bleeding or bruising around the incision
- Feeling or being sick
Serious complications include:- Damage to an internal organ nearby such as bowel, bladder or ureters (urine tubes) during the operation
- Clots in leg or lung
- Heavy bleeding during operation
Which gynaecological procedures are performed with laparoscopy?- Ovarian operations such as ovarian cyst/tumour removal, treatment of PCOS, oophorectomy for tumour or cancer risk reduction
- Fallopian tube procedures such as clip ligation (permanent contraception), removal of tube (ectopic pregnancy and cancer risk reduction)
- Uterine operations such as myomectomy (removal of fibroid) and hysterectomy
- Complex cancer operations such as radical hysterectomy, trachelectomy and lymph node excision
- Investigations and treatment of infertility, endometriosis and pelvic pain
Close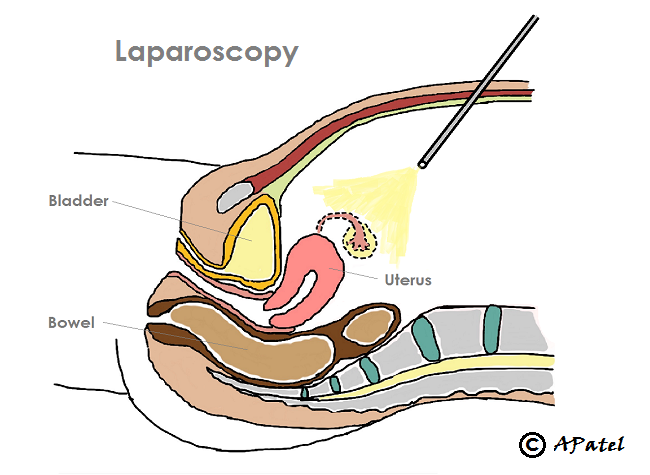
-
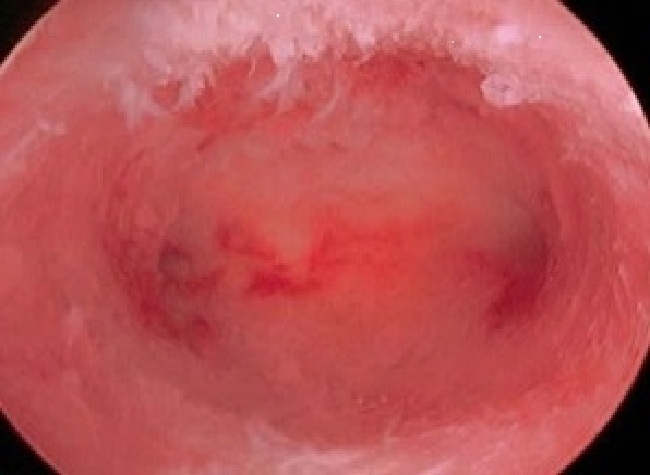
HysteroscopyHysteroscopy is used mainly for the investigation and treatment of irregular or abnormal vaginal bleeding including heavy periods. I hold Royal College of Obstetricians and Gynaecologists (RCOG) specialist qualification in hysteroscopic procedures.More information about hysteroscopy is hereShow meWhat is hysteroscopy?
Hysteroscopy procedure allows visualisation of cervical canal and uterine cavity. It is mainly performed to diagnose cause of irregular periods or vaginal bleeding after menopause. It can also be used to take biopsies, treat polyps or fibroids.
How is it performed?
Simple diagnostic hysteroscopy or minor hysteroscopic procedures can be performed without general anaesthetic in a clinic. Whilst complex cases may require general anaesthetic. Eitherway patient do not need to stay in hospital. After antiseptic preparations vaginal speculum is inserted. Hysteroscope is then passed through the cervix and under image guidance inside uterine cavity. Water or special fluid is irrigated through hysteroscope to dilate uterine cavity and light attached to hysteroscope illuminates uterine cavity. Camera attached to hysteroscope relays images to television screen. Biopsy or removal of polyp or fibroid is then carried out as required.
After the planned procedure is completed, surgeon will ensure that there is no bleeding and will let out the excess fluid.
How long does it take?
Usually it takes about 10 - 30min depending on the aim of procedure.
What are the risks and complications?
Hysteroscopy in gynaecology is a commonly performed procedure and serious complications are very rare.
Minor complications include:- Infection and vaginal discharge
- Minor bleeding afterwards
Serious complications include:- Damage to the uterus or internal organs
Which gynaecological procedures are performed with hysteroscopy?- Biopsy from cervical canal or endometrium (lining of uterine cavity) to rule out cancer
- Removal of polyp or fibroid polyp from cervical canal or uterine cavity
- Ablation of endometrium (treatment of heavy periods)
- Removal of lost coils
Close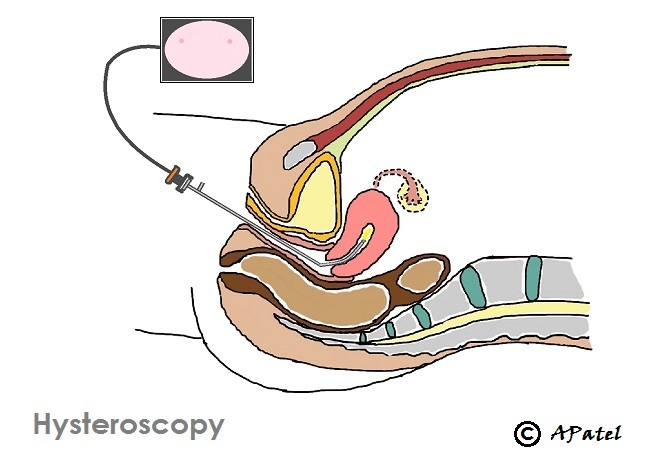
-
ColposcopyColposcopy is used to detect cervical precancer or cancer in women with abnormal smears or abnormal vaginal bleeding. I qualified as a colposcopist from The British Society of Colposcopy and Cervical Pathology (BSCCP) in 2009. I have been performing colposcopy for past 5 years and currently lead the colposcopy department at St. Michael’s Hospital, Bristol. I am also a qualified colposcopy trainer.More information about colposcopy is hereShow meWhat is colposcopy?
A colposcopy is an examination to find out if there are precancerous or cancerous changes in cervix or vagina. Colposcopy is performed if women have abnormal bleeding, abnormality on cervical smear or if there are abnormal changes seen during examination by a GP.
How is it performed?
Colposcopy and colposcopic procedures are usually carried out in clinic and do not require general anaesthetic. After antiseptic preparations vaginal speculum is inserted and cervix is exposed. Colposcope is then used to magnify cervix. Light attached to colposcope illuminates cervix and vaginal surface. Camera attached to colposcope can relays images to television screen. Acetic acid and/or Lugol’s iodine solution is then used help identify abnormal areas in the cervix.
Small diagnostic (punch) biopsy, Loop (LLETZ) biopsy or removal of polyp is then carried out depending on the findings of the colposcopic examination. Local anaesthetic injection is used for loop biopsy and occasionally for the removal of polyp.
How long does it take?
Colposcopy usually takes about 10mins but if loop biopsy is required it can take additional 10mins.
What are the risks and complications?
Colposcopy is a very commonly performed procedure and complications are very rare.
Minor complications include:- Infection and vaginal discharge
- Minor bleeding
Serious complications are rare include:- Heavy bleeding during or after loop biopsy
Which gynaecological procedures are performed with colposcopy?- Cervical cancer screening smear test
- Small punch biopsy from vaginal or cervical surface
- Large loop (LLETZ) biopsy to remove abnormal precancerous area from cervix
- Removal of cervical polyp
- Ablation of vaginal precancerous changes (requires general anaesthetic)
Close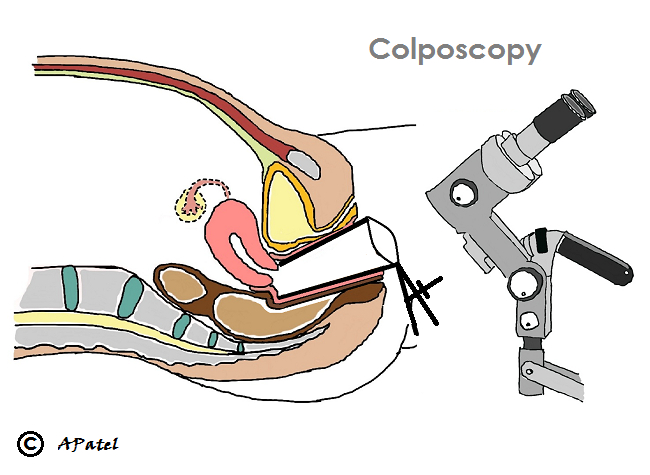

-
Vulvoscopy and vulval diseasesVulval skin diseases can be quite debilitating. Vulvoscopy is similar to colposcopy and is used to rule out vulval skin precancer or cancer. I hold specialist qualification in vulval disease through Royal College of Obstetricians and Gynaecologists (RCOG) and have several years of experience in looking after women with vulval precancer and cancer.More information about vulvoscopy is hereShow meWhat is vulvoscopy?
A vulvoscopy is an examination of vulval skin performed using colposcope to investigate vulval diseases and problems including precancer and cancer of vulva. Vulvoscopy is performed if women have vulval soreness, itching, bleeding or abnormal lump.
How is it performed?
Vulvoscopy is usually carried out in clinic and do not require general anaesthetic. After antiseptic preparations colposcope is used to to magnify vulval skin. Light attached to colposcope illuminates vulval skin and camera attached to colposcope can relays images to television screen. Acetic acid and/or Lugol’s iodine solution may be used to identify abnormal areas in vulval skin.
Small diagnostic (punch) biopsy may be carried out depending on the findings of the vulvoscopic examination. Local anaesthetic injection is used prior to taking biopsy.
How long does it take?
Vulvoscopy usually takes about 5mins but if vulval biopsy is required it can take additional 10mins.
What are the risks and complications?
Vulvoscopy is a very simple examination and do not have any major risk. If biopsy is taken, rarely, women may experience minor bleeding or infection
Which gynaecological procedures are performed with vulvoscopy?- small punch biopsy of vulval skin
Close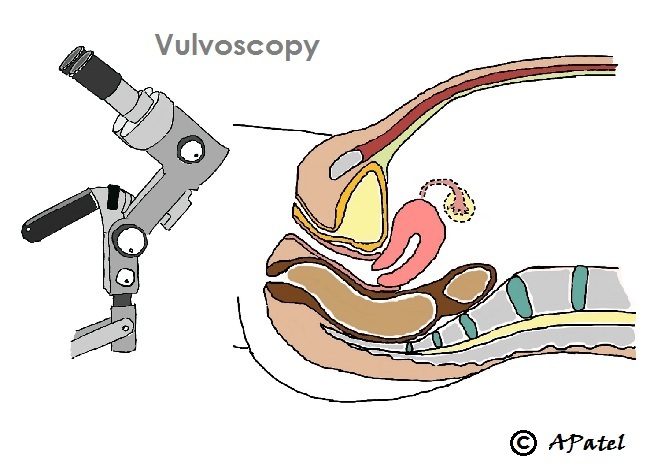

-
Gynaecological CancersMy main expertise through higher specialty training is in confirmed or suspected gynaecological pre-cancer and cancer. I hold the General Medical Council and the Royal College of Obstetricians and Gynaecologists (RCOG) sub-specialty accreditation in gynaecological cancer. These was achieved through a RCOG approved research and clinical training over 6 years. The experience gained over years allows me to offer patient care and advice on range of gynaecological cancer related subjects including screening, prevention, diagnosis, treatment and living with and beyond cancer.For more information about gynaecological cancer - use these links
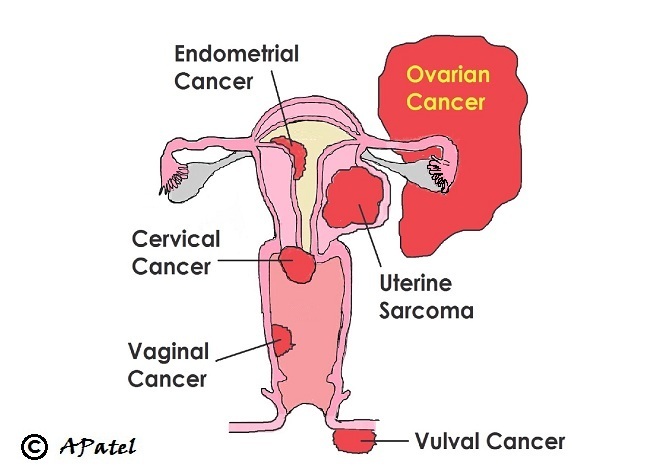

-
Cancer Screening, Risk Reduction and Fertility Sparing TreatmentCancer screening is testing healthy people for signs of a pre-cancer or an early stage of cancer. Aim of screening is to prevent development of a cancer or to catch it in an early stage.
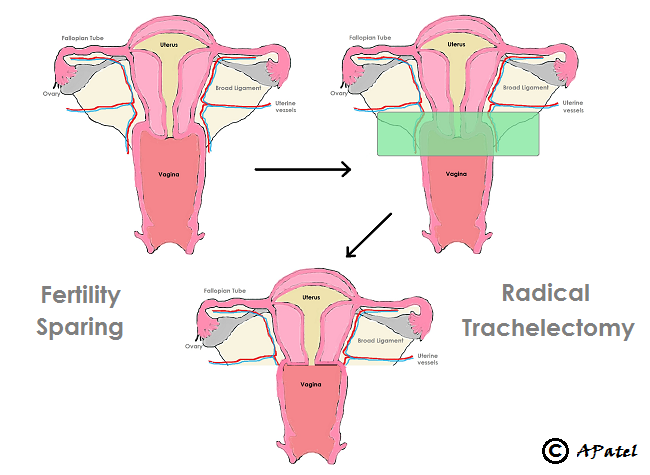
Risk reduction refers to taking an action to reduce the risk of development of cancer in healthy people.More information about Screening and Risk Reduction is hereFertility: Some gynaecological cancers are common at younger age (for e.g. cervical cancer) and there is also a trend towards younger age of onset in many gynaecological cancers. Many women are also choosing to delay their pregnancies to a later age. Fertility therefore can be an important issue when women of reproductive age group is diagnosed with a cancer.
Most treatment of gynaecological cancers have an adverse effect on the fertility. Fertility however can be conserved or preserved in most cases. It is generally easier to do so in early stages of gynaecological cancer. Options available to women are dependant on keen desire to retain fertility, stage of cancer and risk of cancer recurrence. Decisions are very much individualised, discussions are complex and the process can be quite emotional.More information about Fertility options with diagnosis of cancer is here
Open all Close all
-
Conditions I treat …
- Cervical cancer screening and colposcopy
- Irregular bleeding (Postmenopausal, post-coital and persistent inter menstrual bleeding)
- Vulval skin conditions
- Tumours, pre-cancers and cancers of ovaries, fallopian tubes, uterus, cervix and vulva-vagina
- Cancer risk reducing treatment for women at higher risk
- Fertility sparing treatment of precancer and cancer
-
Procedures I offer …Investigations
- Cervical cancer screening (smear) test
- Colposcopy (examination of cervix +/- biopsy)
- Hysteroscopy (examination of inside of womb +/- biopsy)
- Vulvo-vaginoscopy (examination of vulval-vaginal skin +/- biopsy)
- Laparoscopy (examination of inside of abdomen and pelvis +/- biopsy)
Therapeutic
(Most of the major operation are performed as a key-hole surgeries. This allows the best chance of uneventful and quick post-operative recovery.)- Loop biopsy (LLETZ) of cervix
- Hysteroscopy + Polyp removal
- Vulval skin excision
- Advanced laparoscopic (key-hole) surgery (including removal of tubes and ovaries, hysterectomy, radical hysterectomy, trachelectomy (removal of cervix), pelvic and para-aortic lymph nodes)
- Laparotomy (Cut - mainly for large tumours that can not be removed through key-hole)
Open all Close all
© Amit Patel, Bristol
Page last updated - Sept 2016
Site last updated - Aug 2016
