Fertility Options Vs. Cancer Treatments

Some gynaecological cancers are common at younger age (for e.g. cervical cancer) and there is also a trend towards younger age of onset in some gynaecological cancers. Many women are also choosing to delay their pregnancies to a later age. Fertility therefore can be an important issue when women of reproductive age is diagnosed with a cancer.
If fertility is an issue, please discuss this with your doctor as soon as possible.
Most treatment of gynaecological cancers have an adverse effect on the fertility. Fertility however can be conserved or preserved in most cases. It is generally easier to do so in early stages of gynaecological cancer. Options available to the patient are dependant on keen desire to retain fertility, stage of cancer and risk of cancer recurrence. Decisions are very much individualised, discussions are complex and the process can be quite emotional.
Effect of cancer treatment on fertility:
Ovaries contain a fix number of eggs. All the eggs women will ever have are present in the ovaries at birth. Women are not able to grow new eggs. Uterus provides space and environment for the fertilised ovum to grow for nine months.
Cancer treatments with surgery, chemotherapy and radiotherapy can adversely affect the eggs and/or uterus leading to sub fertility or infertility. Removal of ovaries or radiation affecting ovaries can also lead to premature menopause.
Chemotherapy can damage eggs, ovaries and hormone production required for pregnancy. Radiation can damage ovaries and uterus if these are exposed to radiation field. Surgery for gynaecological cancer may require removal of ovaries and/or uterus.
Not all women have their fertility compromised after one of these treatments. Actual effect on fertility depends on many factors such as…
Fertility options available to gynaecological cancer patient:
Delay in cancer treatment:
Fertility options requiring ovulation induction (such as egg or embryo freezing) can take time and therefore may delay the start of cancer treatment. This is usually not very long and harm due to delay is generally very minimal.
Chances of successful pregnancy:
These depends on type of treatment and can be different in each individual even with same treatment. In general there is some reduction in rate of successful pregnancy compared to normal population.
After completion of cancer treatment:
Not all women with gynaecological cancer have their fertility compromised after treatments. If your periods continue or return after treatment it does not always mean that fertility is not affected or has returned.
After completion of treatment and before trying for a pregnancy it is necessary to reassess and thoroughly consider likelihood and implications of cancer recurrence and issues of prognosis and child care in such situation. Even if all is well after treatment, it is generally advisable to wait for about 3 months before trying for a pregnancy.
Pregnancy after cancer treatment:
Depending on the type and radicality of treatment, risk of miscarriages and pre-term births may be higher than normal population. There is no evidence to support that the cancer treatment affects development of foetus or causes foetal anomaly. There is also no evidence that pregnancy increases risk of cancer recurrence.
If fertility is an issue, please discuss this with your doctor as soon as possible.
Most treatment of gynaecological cancers have an adverse effect on the fertility. Fertility however can be conserved or preserved in most cases. It is generally easier to do so in early stages of gynaecological cancer. Options available to the patient are dependant on keen desire to retain fertility, stage of cancer and risk of cancer recurrence. Decisions are very much individualised, discussions are complex and the process can be quite emotional.
Effect of cancer treatment on fertility:
Ovaries contain a fix number of eggs. All the eggs women will ever have are present in the ovaries at birth. Women are not able to grow new eggs. Uterus provides space and environment for the fertilised ovum to grow for nine months.
Cancer treatments with surgery, chemotherapy and radiotherapy can adversely affect the eggs and/or uterus leading to sub fertility or infertility. Removal of ovaries or radiation affecting ovaries can also lead to premature menopause.
Chemotherapy can damage eggs, ovaries and hormone production required for pregnancy. Radiation can damage ovaries and uterus if these are exposed to radiation field. Surgery for gynaecological cancer may require removal of ovaries and/or uterus.
Not all women have their fertility compromised after one of these treatments. Actual effect on fertility depends on many factors such as…
- Site of cancer
- Stage (spread) and grade (aggressiveness) of cancer
- Radicality and type of treatment required
- Age and previous fertility problems
Fertility options available to gynaecological cancer patient:
- Fertility sparing surgery: If uterus and at least one ovary and fallopian tube can be spared during surgery, fertility can be maintained. For example removal of single ovary and fallopian tube in early stage ovarian cancer or removal of just cervix in early stage cervical cancer.
- Ovarian transposition: Ovaries are lifted out of pelvic radiation field by performing small laparoscopic (key-hole) surgery prior to radiation treatment. They can be later used to induce ovulation. Harvested eggs are fertilised and transferred in uterus of a patient (where possible) or a surrogate.
- Egg or embryo freezing: Prior to cancer treatment ovaries are stimulated with ovulation induction treatment and eggs are collected. They are either frozen as eggs or as embryos after fertilisation. They can be used later in a patient (where possible) or in a surrogate.
- Ovarian tissue freezing: Small portion of ovarian tissue is removed and frozen and later re-implanted (for e.g. on arm) and is stimulated for ovulation. Ovum is harvested, fertilised and transferred in uterus of a patient (where possible) or a surrogate.
- Donor eggs: If both ovaries are involved in cancer or removed without possibility of egg or embryo freezing, donor eggs can be used to create embryos which can then be transferred in patient herself (where possible) or in a surrogate.
- Surrogacy: If uterus is affected by cancer treatment or removed during surgery, embryo using either eggs from patient or from egg donor can be implanted in a surrogate uterus. Surrogacy can be achieved by natural fertilisation of surrogates own eggs and patient’s partner’s semen. This requires artificial insemination (transfer of semen using syringe) at right time.
- Hormonal treatment: Endometrial cancer of low grade and low stage can be treated by hormonal treatment such as Insertion of Mirena(R) IUS or high-dose progesterones.
- Uterine transplantation: This is very new technique, mostly used in research settings and is not suitable in most cancer cases. It may be of use in future, particularly in endometrial cancer patients.
- Adoption
Delay in cancer treatment:
Fertility options requiring ovulation induction (such as egg or embryo freezing) can take time and therefore may delay the start of cancer treatment. This is usually not very long and harm due to delay is generally very minimal.
Chances of successful pregnancy:
These depends on type of treatment and can be different in each individual even with same treatment. In general there is some reduction in rate of successful pregnancy compared to normal population.
After completion of cancer treatment:
Not all women with gynaecological cancer have their fertility compromised after treatments. If your periods continue or return after treatment it does not always mean that fertility is not affected or has returned.
After completion of treatment and before trying for a pregnancy it is necessary to reassess and thoroughly consider likelihood and implications of cancer recurrence and issues of prognosis and child care in such situation. Even if all is well after treatment, it is generally advisable to wait for about 3 months before trying for a pregnancy.
Pregnancy after cancer treatment:
Depending on the type and radicality of treatment, risk of miscarriages and pre-term births may be higher than normal population. There is no evidence to support that the cancer treatment affects development of foetus or causes foetal anomaly. There is also no evidence that pregnancy increases risk of cancer recurrence.
-
Ovarian CancerIn early stage of cancer where tumour is only involving one ovary, it is possible to retain fertility by conserving healthy ovary, fallopian tube and uterus. Egg, embryo or ovarian tissue freezing can also be used in such cases.
In advanced cancer where both ovaries are involved in cancer it is generally not advisable to leave uterus or ovaries during surgery. Donor eggs with surrogacy and adoption are the only viable options. Also prognosis of advanced cancer should be thoroughly considered in making decisions regarding treatment options and fertility. -
Uterine CancerIn early stage low grade endometrial cancer fertility can be conserved by combination of conservative surgery (endometrial curettage) and hormonal (progesterone) treatment. There is an emerging evidence of success. That been said there is still a significant risk of sub-optimal cancer treatment and therefore due diligence is required. If such fertility sparing treatment is commenced, women are advised to complete family as soon as possible and then should undergo standard cancer treatment.
In advanced stage or high grade uterine cancer surrogacy with patients own eggs (where possible) or donor eggs and adoption are the only viable options. -
Cervical CancerAs cervical cancer is commonly diagnosed in young women, fertility is often an issue.
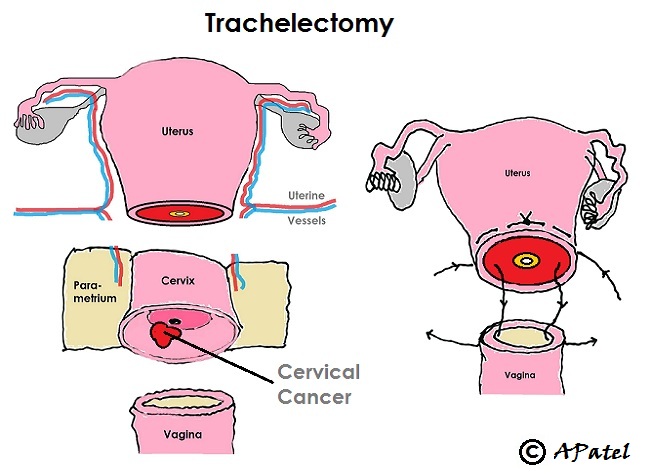
In early stage of cervical cancer (limited to cervix) fertility can be conserved by either loop treatment (for small cancer) or by performing trachelectomy operation (for larger cancer). Loop treatment removes portion of cervix including cervical cancer whilst trachelectomy removes whole of cervix with upper vagina and attached tissue on both side followed by implantation of uterus back onto vagina.
More advanced cervical cancer are generally treated with chemo-radiation treatment. Ovarian transposition prior to radiation may allow surrogacy with patients own eggs. If ovaries are likely to be healthy but can not be spared during surgery or radiation, egg, embryo or ovarian tissue freezing is advisable which can later be used for surrogacy. Donor eggs with surrogacy or adoption are only options if ovaries are involved in cancer or can not be used for any other reason. -
Vulval CancerVulval cancer is rare in young women of reproductive age-group. Fertility is generally not compromised by vulval cancer treatment in most cases as these are managed by surgery that do not affect uterus, ovaries or fallopian tubes.
Radiation to groins if required can be given sparing ovaries or by performing ovarian transposition prior to radiation.
Open all Close all
© Amit Patel, Bristol
Page last updated - Sept 2016
Site last updated - Aug 2016
