Surgical complications
My interest in surgical excellence and patient safety goes long way back.
I have collected data on my own surgical (obstetrics and gynaecology) outcomes ever since I was trainee (Since 1998). This has been an extremely useful activity to improve my surgical skills and patient safety.
Since 2008, I have more detailed data on surgical outcomes which I have voluntarily collected and analysed. These are shared openly below where you will find rates of serious complication associated with a major gynaecological surgery performed by me.
Some facts about gynaecological operations and risks:
Since 2008, I have more detailed data on surgical outcomes which I have voluntarily collected and analysed. These are shared openly below where you will find rates of serious complication associated with a major gynaecological surgery performed by me.
Some facts about gynaecological operations and risks:
- Only small number of women with a gynaecological problem require a major operation.
- Most women having gynaecological operation recovers well without any complications.
- All surgical procedures carry some risk.
- Surgical risks can be minimised but can not be entirely eliminated.
- Individual risks can be estimated but can not be precisely predicted.
- Surgical risks are dependent on several factors including expertise and experience of surgeon, nature of the clinical problem, patient fitness and hospital resources.
- All surgeons are not same.
- It is perfectly ok to ask surgeons about their complication rate.
Analyses of complication rates is an extremely complex process.
Why?
Several factors affect the rate of complication. Some are outlined below …
- Quality of data (e.g. Definition of complications, details, the way and by whom data is collected)
- Completeness of data (e.g. Failure to record known and unknown complications. Patient attending different hospital after discharge)
- Pre-existing co-morbidities (e.g. Young fit vs. old frail patients)
- Expertise of surgeon (e.g. Training, experience, workload and ability to self-criticise)
- Level of risk aversion (e.g. Surgeons offering operations to high-risk patient have a higher complication rates)
- Complexity of pathology (e.g. Benign vs. cancer conditions)
- Complexity of procedure (e.g. First operation vs. multiple previous operations)
- Hospital resources (e.g. availability of advanced technology and instruments)
Close
My outcomes (This is still a work in progress, please check again little later)
The data and method used to calculate my outcomes are described here.
(To understand the full context of the results below, I would recommend reading this.)
(To understand the full context of the results below, I would recommend reading this.)
Lets see
Data and Method:
- Includes all records available from 2008 - until the date this page is updated
- All major laparotomy (cut) and laparoscopy operations (key-hole) operations (analysed separately) are included
- Minor operations such as biopsies, small procedures, diagnostic procedures and vulvo-vaginal procedures are excluded
- Only operations performed by myself are included
- My results are compared against the rates published in medical literature by other gynaecological oncologists
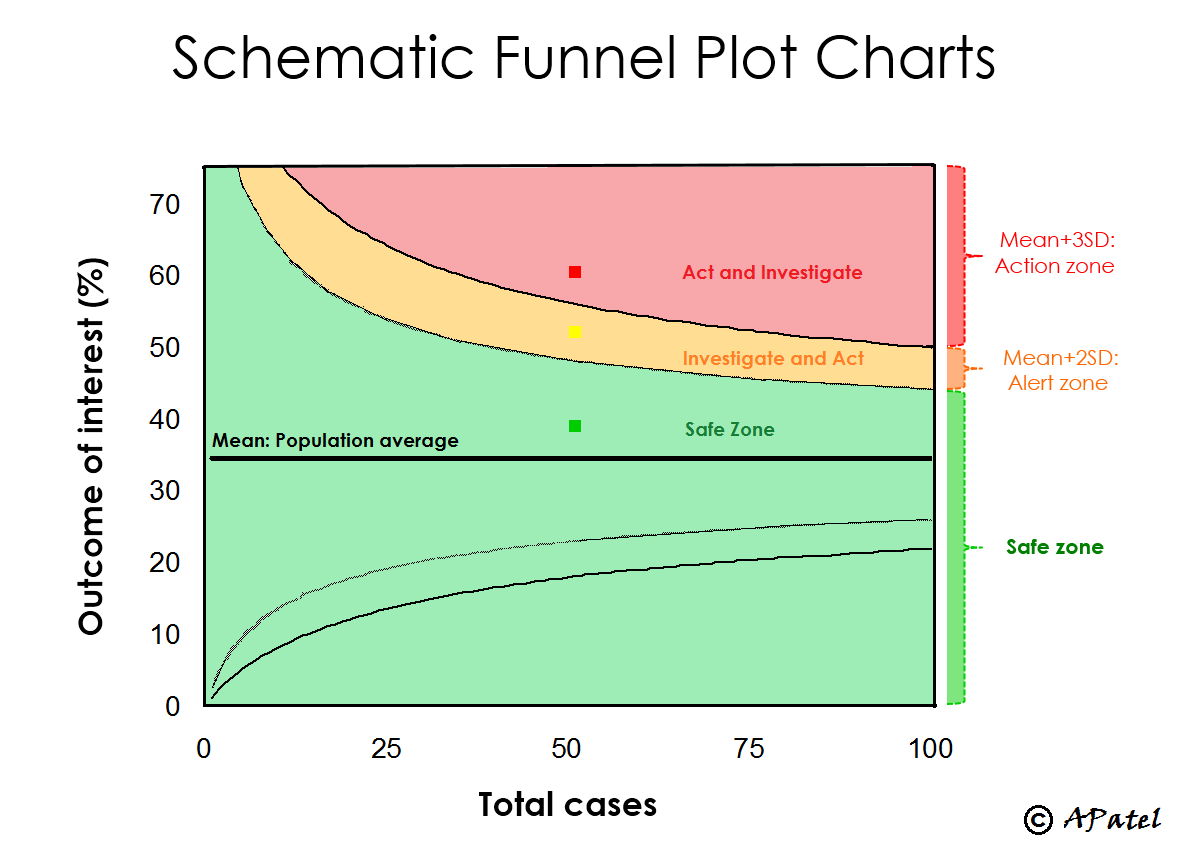
- Each graph has middle straight line representing Mean (published rate in literature), Marker (my rate), Alert and Action lines above mean (representing significantly higher rate than expected that requires alert and action if marker crosses these lines). See figure below …
Close
-
Intra-operative: Damage and Injury Rate
-
Intra-operative: Heavy bleeding (> 2 litre) and blood transfusion rate
-
Post-operative: Unplanned Return to Theatre (within 30 days)
-
Post-operative: Death (within 30days)
Open all Close all
© Amit Patel, Bristol
Page last updated - Sept 2016
Site last updated - Aug 2016
