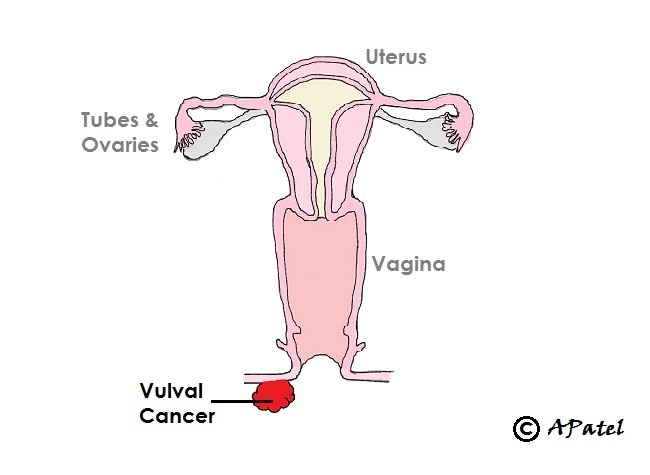
Vulval Cancer
-
Statistics
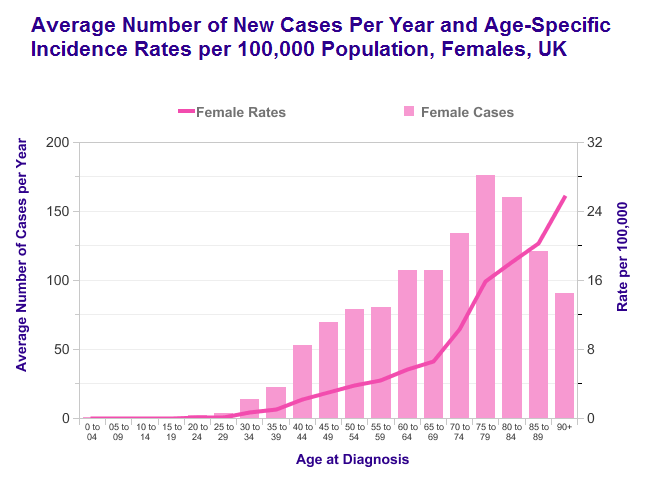
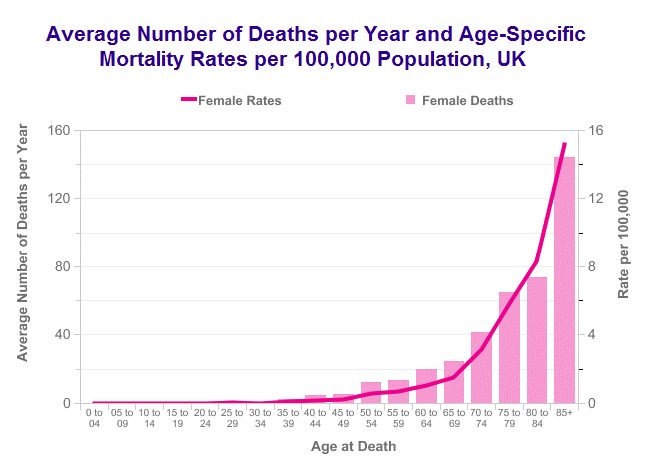
- 1,300 new cases per year in UK
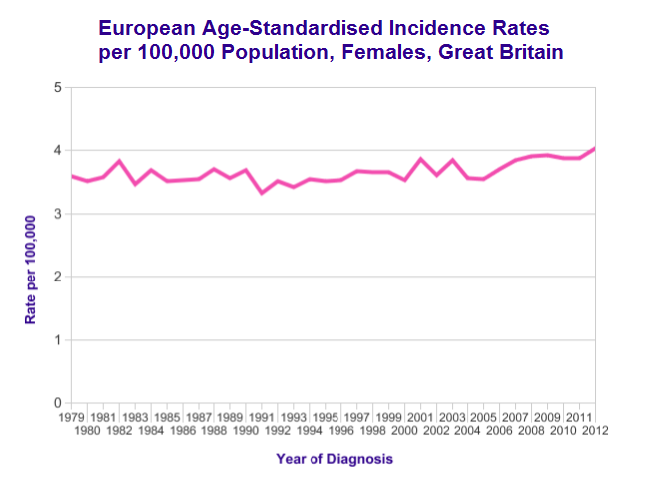
- 4 cases per 100,000 women per year in UK
- Life-time risk of 1 in 275
- >50% cases are in women aged over 70 years
- 9 out of 10 cases are Squamous Cell Cancer type
- Incidence has not changed much over years
-
Risk factors and Causes
- Age
- Human papillomavirus (HPV)
- Human immunodeficiency virus (HIV)
- Previous cervical, vaginal, anal or oro-pharyngeal cancer
- Untreated high-grade vulval intraepithelial neoplasia (VIN)
- Chronic skin conditions (Lichen sclerosus, Lichen planus, Paget's disease)
- Auto-immune conditions (systemic lupus erythematosus (SLE) or psoriasis)
- Solid organ transplant recipients
- Tobacco usage
-
ScreeningThere is currently no population screening programme for vulval cancer.
However during cervical cancer screening test (smear test), the nurse or doctor may routinely examine vulval skin.
Women with higher risk such as chronic skin conditions (for e.g. Lichen Sclerosus) or precancerous conditions (VIN) may benefit from regular vulval skin examinations. -
Symptoms
- Itching
- Vulval pain or soreness
- Red, white or dark, thickened or raised, vulval skin patches
- Vulval skin ulcer
- A lump or tumour
- Bleeding from vulval skin
-
InvestigationsFor Diagnosis
- Vulvoscopy and/or vulval skin examination
- Excision or punch biopsy of the vulval lesion
For Staging- Examination under anaesthetic with cystoscopy (camera check of inside of bladder) and rectal examination if tumour extension to urethra, bladder or back-passage is suspected
- CT scan and/or MRI to check for cancer spread to lymph nodes and other parts of body
-
FIGO StageStage 1 – Cancer is limited to the vulval skin
Stage 2 – Cancer has spread to nearby parts such as the lower vagina, anus or lower urethra (the tube urine passes through out of the body)
Stage 3 – Cancer has spread into groin lymph nodes
Stage 4 – Cancer has spread to upper urethra, upper vagina, back-passage lining or other parts of the body -
TreatmentSurgery
Surgery is the main treatment for vulval cancer.
1. Vulval tumour removal:
Depending on the size of tumour wide local excision (commonly), partial vulvectomy, radical vulvectomy (rarely) is required. Aim of surgery is to remove tumour with healthy with healthy margin.
Some women with advanced cancer where cancer is close to or involving anal skin may also require removal of anal opening (ano-vulvectomy) and diversion of bowel with colostomy. This however is rarely required.
2. Lymph node spread assessment:
In most women (except for very early stage of cancer) assessment of one or both side of groin lymph nodes for cancer spread is also required. Groin lymphadenectomy operation is aimed to remove all lymph nodes from the groin. This operation has high rate of side-effect such as wound breakdown, leg swelling and groin lymph cyst formation.
To avoid such side effects, some women who are eligible (with single tumour of less than 4cm size) may be offered Sentinel lymph node detection technique. Sentinel node is the key lymph node among all other groin nodes. Dye injection is used to identify sentinel lymph node. Once identified, removed, checked and if found negative there is more than 95% chance that other groin nodes are negative too. This avoids removal of all other nodes and associated major side effects of operation.
Radiotherapy and Chemotherapy
After operation if lymph nodes are found positive further treatment with radiotherapy may required. Chemotherapy may also be used to improve the success of radiothearpy to cancer.
Women who are not fit for surgery or those with advanced stage of cancer may also be treated radiotherapy, chemotherapy or combination. -
SurvivalSurvival in vulval cancer mainly depends on the
- FIGO stage of the cancer (how far has cancer spread)
- Grade of cancer (how aggressive cancer cell look under microscope)
- Morphology (cell type) of cancer
- Age
- Fitness of patient
In general at least 60 out of 100 women with vulval cancer will live 5 years or more.
Survival has improved continuously over decades.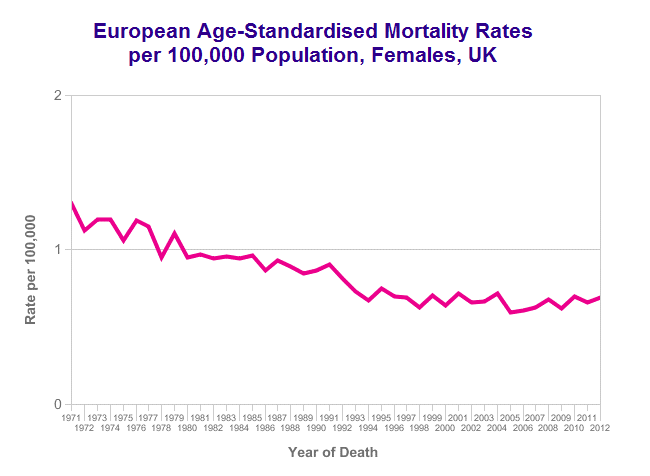
Open all Close all
References:
- Cancer Research UK, http://www.cancerresearchuk.org/health-professional/vulval-cancer-statistics, Accessed Feb 2016
- NHS Choices UK, http://www.nhs.uk/Conditions/Cancer-of-the-vulva/Pages/Introduction.aspx, Accessed Feb 2016
© Amit Patel, Bristol
Page last updated - Sept 2016
Site last updated - Aug 2016
